
2022 Post-doctoral Clinical Fellowship
Investigating the relationship between CSF drainage and measures of peripheral and central inflammation in Parkinson’s disease
I am a neurologist and am interested in how the immune system affects progression in Parkinson’s disease. In the last decade, there is increasing evidence that the immune cells in the meninges (the covering around the brain) and skull bone marrow are also important for brain health. Currently we have no therapies to halt the progression of Parkinson’s disease or prevent complications such as dementia and balance problems. Understanding more about how the immune system interacts with the brain in diseases like Parkinson’s disease will help us to identify drugs that might be able to prevent these complications.
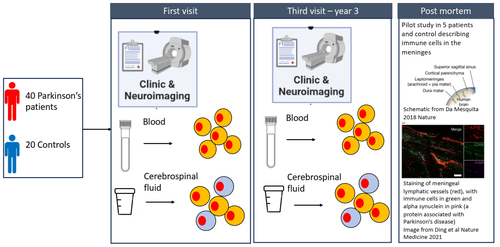
I am going to analyse data from a longitudinal study run by Caroline Williams-Gray, the NET-PDD study, where we have MRI scans and PET scans (a scan using a radioactive substance that binds to immune cells in the brain) from 40 patients and 20 controls at baseline and again three years later. These scans can give us information about the microglia, the predominant immune cell in the brain, immune cells in the skull and estimates of the drainage of the fluid around the brain. The patients also gave blood and cerebrospinal fluid (CSF). We have used flow cytometry to characterise immune cells in these patients in blood and CSF. I am going to see whether there is a relationship between some imaging markers of inflammation and changes in the blood and whether either of these relate to changes in drainage of cerebrospinal fluid or to the immune cells in the CSF. We can also look at whether any of these are associated with progression of disease. I am also going to look at immune cells in the meninges from our brain bank in a small descriptive pilot study to see whether we can see similar changes to those described in mouse models.
Follow up after fellowship:
Kirsten joined AstraZeneca in 2023 as Medical Director, Neurosciences , R&D Biopharmaceuticals. Following restructuring in AstraZeneca, Kirsten took up a position as Clinical Lead in AC Immune, a biotech company based in Lausanne, Switzerland.